Introduction to the e-STAR Program
Understanding the FDA e-STAR Program: Your Roadmap to Compliance
What is the FDA e-Star Program?
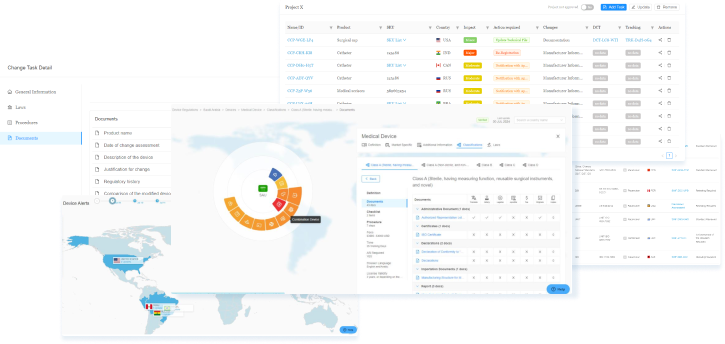
The healthcare landscape continues to evolve rapidly, demanding innovative solutions to maintain safety, efficiency, and speed in regulatory processes. To meet this need, the U.S. Food and Drug Administration (FDA) has developed the e-STAR (Electronic Submission Template and Resource) program, a tool that helps streamline premarket submissions for medical devices. Launched as a part of the FDA’s broader digital initiatives, e-STAR reduces manual entry, integrates error-checking, and simplifies documentation, directly benefiting regulatory professionals and manufacturers alike (FDA, 2023a). By simplifying the complex premarket submission process, e-STAR facilitates faster device reviews while maintaining the rigor needed for public safety.
Overview of the FDA’s e-STAR Program
The e-STAR program addresses the historically complex nature of FDA’s medical device submission processes. Submissions for medical devices often require extensive documentation, including detailed descriptions, risk analyses, clinical data, and manufacturing processes. Given this complexity, submissions often faced delays due to minor errors or omissions. e-STAR tackles these challenges by offering a step-by-step template that aligns with regulatory requirements, reducing errors and facilitating a more seamless submission experience (FDA, 2023b).
Structure and Components of the e-STAR Template
Device Information and Intended Use
Each e-STAR submission begins with a thorough overview of the device’s basic information, including device type, intended use, and classification. This section helps applicants clearly define the scope and purpose of their device, ensuring FDA reviewers understand its function and risk profile. By standardizing this step, e-STAR reduces ambiguity in device categorization, setting the stage for a more efficient review (FDA, 2023c).
Design Verification and Validation
Quality Systems Compliance
The Role of e-STAR in FDA’s Digital Transformation
Streamlining Premarket Submissions
Enhanced Review Efficiency
Traditionally, the FDA’s review process for 510(k) clearances and Premarket Approval (PMA) applications required considerable time due to lengthy submissions and variable documentation standards. With e-STAR, applicants benefit from predefined fields and prompts, ensuring that submissions align more precisely with FDA requirements. By reducing redundant information and minimizing formatting errors, e-STAR enables FDA reviewers to access the information they need more quickly, which leads to shorter review times and faster market entry for medical devices (FDA, 2023d).
Transparent Submission Process
Case Study: 510(k) Submissions with e-STAR
For example, many companies that use e-STAR for 510(k) submissions have reported significant reductions in review times due to the template’s structured format. A typical 510(k) submission involves documenting substantial equivalence to a predicate device, which can be complex if not organized effectively. e-STAR’s template clarifies the requirements for demonstrating substantial equivalence, supporting applicants in preparing comprehensive and clear submissions. FDA reviewers benefit as well, as e-STAR enables them to quickly compare the new device with its predicate, thereby speeding up the review process and contributing to reduced overall timelines (Patel, 2022).
Types of Medical Devices Covered: Device Classifications and e-STAR Submission Processes
Classifications of Medical Devices and Their Requirements
Class I Medical Devices (Low Risk)
Class I medical devices are considered low-risk and generally do not support or sustain life. They include simple items often used in routine medical care, such as bandages, examination gloves, manual stethoscopes, and tongue depressors. Since these devices pose minimal risk, the FDA applies the least stringent regulatory controls. While most Class I devices are exempt from premarket notification (510(k)), they must still meet FDA’s general controls, which include requirements for labeling, manufacturing practices, and record-keeping.
Regulatory Requirements for Class I Devices
General Controls: These include standards for device registration, labeling, record-keeping, and adherence to Good Manufacturing Practices (GMP). Manufacturers must ensure their devices are safe and comply with general controls, which are foundational regulatory requirements.
Exemptions from Premarket Review: Because of the low risk, many Class I devices are exempt from the 510(k) premarket notification, reducing the burden on manufacturers and allowing faster market entry.
e-STAR Support for Class I Devices
Streamlined Documentation: e-STAR offers templates that help manufacturers complete required documentation for Class I devices, covering essential information on device labeling and GMP compliance. This reduces the time and effort needed to meet FDA expectations.
Error-Checking Features: Even though Class I devices have fewer regulatory requirements, e-STAR’s error-checking functions help manufacturers ensure that their submissions are accurate and complete, reducing the likelihood of delays.
Class II Medical Devices (Moderate Risk)
Class II medical devices present moderate risk and require additional regulatory oversight to ensure safety and effectiveness. This category includes devices like diagnostic imaging systems, infusion pumps, and powered wheelchairs. Most Class II devices require a 510(k) submission to demonstrate substantial equivalence to an already approved device. This requirement ensures that the device performs as safely and effectively as similar devices already on the market.
Regulatory Requirements for Class II Devices
510(k) Submission for Substantial Equivalence: Manufacturers must show that their device is substantially equivalent to a legally marketed device (predicate). The 510(k) submission includes detailed documentation, such as device description, intended use, performance testing data, and labeling.
Special Controls: In addition to general controls, some Class II devices must meet specific regulatory standards, known as special controls. These controls may include requirements for additional testing, specific labeling, and post-market surveillance.
Template for Substantial Equivalence: e-STAR guides manufacturers through the substantial equivalence demonstration by organizing data fields for comparisons with predicate devices. This includes sections for device design, testing, and intended use, all critical for establishing equivalency.
Automated Validation: e-STAR’s error-checking system ensures that each section is completed, reducing the likelihood of incomplete or inconsistent submissions that could delay the FDA review process.
Clarity and Standardization: With e-STAR’s standardized template, manufacturers can provide clear, consistent information. This approach minimizes errors and misunderstandings, allowing FDA reviewers to assess 510(k) applications more efficiently.
Class III Medical Devices (High Risk)
Class III medical devices represent the highest-risk category, usually life-supporting or life-sustaining, and are subject to the most rigorous regulatory requirements. These devices include products like pacemakers, artificial heart valves, and implantable defibrillators. Due to the high stakes associated with their use, most Class III devices must undergo the Premarket Approval (PMA) process, which involves comprehensive testing and clinical trials to establish safety and efficacy.
Regulatory Requirements for Class III Devices
PMA Submission: PMA applications require extensive data, including preclinical and clinical trial results, design and manufacturing information, and a detailed risk-benefit analysis. The FDA’s review process is thorough, ensuring the device meets the highest standards of safety and effectiveness.
Risk Management Documentation: Manufacturers must submit risk assessments, outlining potential hazards and mitigation strategies. This is critical for devices that pose significant health risks if they malfunction.
Quality System Regulation Compliance: Compliance with the Quality System Regulation (QSR) is mandatory, verifying that the device meets FDA’s standards for manufacturing and quality control.
e-STAR’s Role in Facilitating PMA Submissions
Data Organization for Clinical Evidence: e-STAR provides designated fields for clinical trial data, including patient safety and effectiveness results. The program’s structure helps manufacturers present organized, thorough data that FDA reviewers can assess efficiently.
Comprehensive Error-Checking: Given the complexity of PMA applications, e-STAR’s automated error-checking helps manufacturers avoid common mistakes that might otherwise lead to FDA requests for additional information (RAIs).
Structured Submission for Risk Management: e-STAR includes sections for risk assessments and risk mitigation documentation, ensuring all necessary information is available for FDA reviewers to make informed decisions.
Special Submissions: The De Novo Pathway
The De Novo classification is an alternative pathway for moderate-risk devices that lack a legally marketed predicate, allowing novel devices to enter the market without being confined to existing classification frameworks. This process enables manufacturers to submit devices that represent significant innovations, especially those that offer new technological advances without fitting within the constraints of traditional classifications.
Regulatory Requirements for De Novo Submissions
- Risk-Based Evidence
De Novo submissions require manufacturers to demonstrate that the device is safe and effective, even though it lacks a predicate device for comparison. This often includes comprehensive performance data, risk assessments, and potentially clinical data if deemed necessary by the FDA.
- Data on Safety and Effectiveness
The FDA expects manufacturers to submit evidence of the device’s safety and effectiveness, tailored to its intended use. This often involves preclinical or clinical data, depending on the device’s nature and risk profile.
e-STAR’s Role in De Novo Submissions
- Flexibility and Adaptability for New Technologies
e-STAR’s templates are flexible enough to support novel devices that do not follow traditional regulatory pathways. Manufacturers can organize data in a way that reflects the device’s unique attributes and intended use, allowing FDA reviewers to understand its novel design and functionality.
- Automated Validation and Error-Checking
e-STAR’s built-in validation and error-checking ensure that De Novo submissions meet all necessary requirements, reducing potential delays due to incomplete or inconsistent information.
e-STAR. A wearable health-monitoring device developer utilizes e-STAR to prepare a De Novo application. With e-STAR’s flexibility, the manufacturer includes sections on device design, functionality, and clinical performance data, offering FDA reviewers a clear understanding of this innovative device’s capabilities. The structured submission format helps reduce review time, facilitating a smoother regulatory process for novel technology.
Streamlined Submission Processes with e-STAR Across All Classifications
e-STAR offers several advantages for each device classification, including structured templates, error-checking mechanisms, and standardized submission formats. By tailoring submissions based on device risk, e-STAR provides a systematic, efficient, and reliable approach to regulatory compliance.
Key Advantages of e-STAR for Each Device Class
Standardization and Clarity: e-STAR promotes uniformity across submissions, making it easier for both manufacturers and FDA reviewers to navigate complex data.
Automated Validation and Compliance Checks
For all device classes, e-STAR includes validation and compliance checks that help manufacturers identify and correct issues early in the submission process.
Support for Innovation
e-STAR’s flexible templates and error-checking capabilities accommodate devices that fall under emerging technology categories, supporting innovation and allowing faster market access for groundbreaking medical products.
Timeline Expectations for Different Medical Devices
510(k) Submissions and Typical Timelines
Standard 510(k) Review Timeline
The FDA’s goal for standard 510(k) submissions is to review applications within 90 days. However, this timeline can vary depending on several factors, such as the quality of the submission, the need for additional data, and the FDA’s current workload.
Factors Influencing the 90-Day Timeline
Requests for Additional Information (RAIs): If the FDA identifies missing or unclear information, they may issue an RAI, which pauses the review clock until the manufacturer provides the necessary information.
Quality and Completeness of the Submission: Submissions using e-STAR benefit from built-in prompts and validation features that help ensure all necessary data is included, reducing the likelihood of RAIs and minimizing potential delays.
e-STAR’s Impact on the 510(k) Timeline
e-STAR’s standardized template and automated error-checking streamline the 510(k) submission process, allowing manufacturers to avoid common pitfalls. By organizing data in line with FDA’s requirements, e-STAR improves submission accuracy and clarity, which can potentially lead to faster review times within or even less than the typical 90-day window.
Special 510(k) and Abbreviated 510(k) Pathways
e-STAR’s standardized template and automated error-checking streamline the 510(k) submission process, allowing manufacturers to avoid common pitfalls. By organizing data in line with FDA’s requirements, e-STAR improves submission accuracy and clarity, which can potentially lead to faster review times within or even less than the typical 90-day window.
Special 510(k) and Abbreviated 510(k) Pathways
In addition to standard 510(k) submissions, the FDA offers two alternative pathways for devices with minor modifications or simplified risk profiles:
- Special 510(k) Submission
This pathway is designed for devices with limited modifications to an existing, previously cleared device. Because it focuses only on the modifications, the review process is often quicker, typically completed within 30 days.
- Abbreviated 510(k) Submission
For devices meeting specific guidance documents or recognized standards, the abbreviated 510(k) allows manufacturers to rely on established standards rather than conducting new testing, expediting the review.
A manufacturer submits a 510(k) application for a modified ultrasound machine, choosing the Special 510(k) pathway. Using e-STAR, they document the modifications clearly, focusing on changes and substantial equivalence to the predicate device. The e-STAR format helps reduce review time, allowing the FDA to approve the device within 30 days.
De Novo Classification and Timeline Considerations
Standard Timeline for De Novo Submissions
The De Novo classification process generally requires 150 to 200 days, due to the FDA’s need to evaluate the safety and effectiveness of a new technology with no predicate for comparison. Factors affecting this timeline include the level of supporting data provided, such as clinical or performance data, and whether additional testing is necessary.
Complexity of Submission and Required Data
De Novo applications require a high level of detail in demonstrating safety and effectiveness, particularly when clinical data is included. This lengthens the timeline compared to 510(k) reviews.
e-STAR’s structured templates help manufacturers present performance and risk assessment data in a way that aligns with FDA requirements, improving submission clarity and potentially reducing review time within the standard window.
e-STAR’s Role in De Novo Submissions
By organizing submission data within the e-STAR framework, manufacturers benefit from standardized fields for risk management, intended use, and safety data. These features help reduce the review time by minimizing ambiguity and facilitating quicker FDA assessments of novel devices.
A company developing a novel wearable ECG monitor opts for the De Novo pathway. Using e-STAR, they compile detailed data on the device’s intended use, performance, and clinical testing. The structured submission format enables the FDA to conduct a clear and efficient review, completing the process within 180 days.
PMA Submissions and Timelines for Class III Devices
Typical PMA Review Timeline
The FDA aims to complete PMA reviews within 180 days, although the actual review period can vary based on device complexity, data volume, and the need for additional clarifications.
The FDA aims to complete PMA reviews within 180 days, although the actual review period can vary based on device complexity, data volume, and the need for additional clarifications.
Factors Affecting PMA Review Timelines
Volume and Complexity of Data
PMA submissions require comprehensive preclinical and clinical evidence, including safety, efficacy, and quality data. Large volumes of clinical trial data can extend the timeline, particularly if there are inconsistencies or gaps.
FDA Requests for Additional Data
If the FDA identifies missing or unclear data, it may issue an RAI, pausing the review until the requested information is provided.
How e-STAR Streamlines PMA Submissions is described as follows, e-STAR’s templates for PMA submissions include fields for clinical trial data, risk management, and quality system compliance, ensuring a well-organized presentation. The standardized format and error-checking functions reduce the chances of incomplete submissions, minimizing delays and supporting FDA’s thorough review process.
Panel Track and Expedited PMA Review Options
Panel Track PMA Supplement
For modifications requiring review by an advisory committee, the Panel Track PMA supplement is a specialized pathway that ensures in-depth evaluation. Although this process is typically lengthy, e-STAR can streamline submission preparation, ensuring that all required data is present and correctly formatted.
Expedited PMA Review for Breakthrough Device
Devices with breakthrough designation may be eligible for an expedited PMA review, allowing critical devices faster access to the market. e-STAR helps these manufacturers prepare comprehensive submissions quickly by automating error-checks and providing pre-set fields for critical safety and efficacy data.
A manufacturer submits a PMA application for a new implantable cardiac device, leveraging the expedited review for its breakthrough designation. Using e-STAR, they submit well-organized clinical trial data and risk assessments. The streamlined format helps FDA reviewers evaluate the data promptly, potentially reducing the review time to under 150 days.
Panel Track and Expedited PMA Review Options
| Device Class | Preparation Phase | Submission | Substantive Review | Final Decision |
| Class I | 1-3 months | Immediate | 90 days | ~90 days |
| Class II | 3-6 months | Immediate | 90 days | ~150 days |
| Class III (PMA) | 6-12 months | Immediate | 180-360 days | 12-18 months |
Expedited Pathways and Their Impact on e-STAR Timelines
Breakthrough Device Designation
Benefits of Breakthrough Designation are as follows,
Devices with breakthrough designation receive prioritized review, which can cut the review time significantly.
The designation provides a pathway for regular FDA feedback during the development process, enabling manufacturers to align their submissions with FDA expectations.
e-STAR’s Role in Supporting Breakthrough Designation is as follows,
e-STAR allows manufacturers to compile complex data efficiently, ensuring that breakthrough devices meet FDA’s expedited requirements. The standardized submission format supports quicker FDA reviews by making critical data accessible and easily navigable.
Emergency Use Authorization (EUA)
EUA Requirements and Benefits
EUA provides a rapid route to market for devices addressing health crises. Devices cleared under EUA can reach patients more quickly than through standard pathways.
e-STAR supports EUA applications by organizing data in alignment with emergency review requirements, enabling a more efficient assessment process.
Case Example
A manufacturer submits a PMA application for a new implantable cardiac device, leveraging the expedited review for its breakthrough designation. Using e-STAR, they submit well-organized clinical trial data and risk assessments. The streamlined format helps FDA reviewers evaluate the data promptly, potentially reducing the review time to under 150 days.
e-STAR’s Role in Reducing Timeline Variability Across Submission Types
- Standardized Templates and Error Reduction
e-STAR’s templates minimize submission errors, improving data clarity and reducing RAIs. This consistency allows the FDA to maintain predictable review timelines across submission types, even for complex PMAs and breakthrough designations. - Pre-Submission Consultations and Feedback
For complex devices, e-STAR facilitates pre-submission meetings with the FDA, allowing manufacturers to align their data with FDA expectations. This proactive approach can reduce review time significantly by addressing potential issues before formal submission. - Consistency in Submission Quality
With e-STAR’s comprehensive structure, manufacturers provide consistent, high-quality data that minimizes variability in review timelines. The program’s standardized approach enhances FDA’s ability to assess and approve safe, effective devices within predictable timeframes.
Example of Improved Consistency with e-STAR
A mid-sized company developing a new Class II medical imaging device submits a 510(k) application using e-STAR. Thanks to e-STAR’s error-checking features, their submission is complete, reducing review time and ensuring predictable timelines despite the FDA’s high workload.
The FDA’s e-STAR program plays a pivotal role in managing and optimizing the timeline expectations for medical device submissions across various pathways, including 510(k), De Novo, and PMA. By providing structured templates, automated validation, and standardization across device classes, e-STAR supports efficient and predictable review processes. Additionally, expedited pathways like breakthrough designation and EUA are enhanced by e-STAR, enabling faster market entry for devices that address critical health needs. Through these innovations, e-STAR improves submission quality, reduces variability in review timelines, and contributes to the FDA’s mission of delivering safe, effective devices to patients in a timely manner.
PMA (Premarket Approval) and Device-Specific Considerations
Overview of PMA and Class III Device Requirements
Data Requirements for PMA Submissions
Clinical Trial Data
Class III devices often require data from human clinical trials, demonstrating safety and effectiveness for the intended use.
Preclinical Testing
PMA applications include data from laboratory and animal studies to show the device’s performance before human testing.
Quality System Compliance
Manufacturers must provide evidence that their quality management system complies with FDA’s Quality System Regulation (QSR) to ensure consistent manufacturing and quality.
Risk Management and Risk-Benefit Analysis
Given the high-risk nature of Class III devices, PMA submissions also require manufacturers to include comprehensive risk management documentation. This documentation outlines potential hazards and mitigation strategies and evaluates the overall risk-benefit profile of the device.
FDA Review Timelines for PMA Applications
The FDA typically aims to review PMA submissions within 180 days, but due to the complex nature of the required data, reviews often extend beyond this timeline. Delays frequently occur due to requests for additional information (RAIs) or clarifications on clinical trial data.
How e-STAR Supports PMA Submissions
Key Features of e-STAR for PMA Submissions
- Standardized Fields for Clinical Data
e-STAR includes specific sections for clinical trial data, allowing manufacturers to present safety and efficacy results in a standardized format. This structure makes it easier for FDA reviewers to locate and analyze essential information, potentially reducing review time. - Risk Management Documentation
e-STAR provides designated fields for risk management, including hazard analysis, mitigation plans, and overall risk-benefit assessments. This structured approach ensures that all necessary risk-related information is included, minimizing requests for additional data from FDA reviewers.
- Automated Validation and Error-Checking
PMA applications involve extensive documentation, and incomplete or inconsistent submissions can cause delays. e-STAR’s automated error-checking function helps manufacturers catch missing or incorrect data before submission, reducing the likelihood of RAIs that could extend the review timeline.
- Organized Quality System Compliance Section
e-STAR provides fields for documenting compliance with FDA’s Quality System Regulation (QSR), allowing manufacturers to showcase adherence to quality management standards. By providing a structured approach to QSR compliance documentation, e-STAR supports FDA’s thorough review of manufacturing quality.
Benefits of Using e-STAR for PMA Submissions
Efficiency in Data Compilation
e-STAR’s template guides manufacturers through each section, making it easier to compile the extensive data required for PMA submissions. This reduces administrative workload and helps ensure that all essential information is included.
Improved Submission Accuracy
By structuring data and incorporating validation checks, e-STAR reduces errors and omissions, increasing the likelihood of a successful first submission.
Enhanced FDA Review Process
e-STAR’s standardized format helps FDA reviewers access key data quickly, improving review efficiency and potentially shortening the approval timeline.
Case Examples of PMA Submissions Through e-STAR
Case Example 1: PMA Submission for an Implantable Cardiac Defibrillator
A medical device company developed a new implantable cardiac defibrillator, a Class III device intended to detect and correct irregular heartbeats in patients at risk of sudden cardiac arrest. Given the high-risk nature of this device, the company needed to submit an extensive PMA application with robust clinical and preclinical data.
- Using e-STAR for Clinical Trial Data
The company used e-STAR’s designated fields to input data from multi-phase clinical trials, including patient safety outcomes, efficacy rates, and device performance metrics. By organizing trial data in e-STAR, the manufacturer ensured a clear, logical presentation, enabling FDA reviewers to assess clinical results more efficiently. - Documenting Risk Management
e-STAR’s template prompted the company to include comprehensive risk management data, detailing potential device failure modes and the steps taken to mitigate these risks. The FDA review team could easily locate and evaluate these risk assessments, which streamlined the review process. - Reduced Review Timeline
Thanks to e-STAR’s structured format and error-checking features, the submission contained all necessary data on the first attempt, reducing the likelihood of RAIs. This organization allowed FDA reviewers to complete the evaluation in under 180 days, allowing the device to reach the market more quickly than anticipated.
Case Example 2: PMA Submission for an Artificial Heart Valve
Another company developed an artificial heart valve, a life-sustaining device for patients with severe heart valve disease. The device required a PMA submission that included preclinical testing, clinical trial data, and quality system compliance documentation.
- Preclinical Testing and e-STAR Support
The manufacturer conducted extensive preclinical testing, including mechanical durability tests, biocompatibility studies, and stress testing. Using e-STAR, they documented these results in designated fields, presenting clear data that aligned with FDA’s review criteria. - Clinical Trial Organization
e-STAR’s template helped the manufacturer organize data from clinical trials involving hundreds of patients. The structured fields allowed for a concise summary of patient safety outcomes, device efficacy, and adverse event rates, making it easier for FDA reviewers to analyze these findings. - Quality System Compliance Section
The company used e-STAR to demonstrate adherence to the Quality System Regulation (QSR) by including data on manufacturing consistency, quality control measures, and corrective action plans. This section helped assure FDA reviewers of the device’s consistent quality and safety. - Outcome
The e-STAR template improved submission clarity, which helped reduce review time. The FDA approved the heart valve within the 180-day review period, allowing the company to proceed to market sooner than expected.
Additional Considerations for PMA Submissions Using e-STAR
- Pre-Submission Consultations with FDA
Engaging in pre-submission meetings with the FDA can help manufacturers align their PMA applications with FDA expectations. These consultations provide an opportunity to discuss data requirements, address potential concerns, and ensure that the e-STAR template will effectively support the device’s unique characteristics. - Comprehensive Clinical Data Presentation
For devices requiring rigorous clinical testing, e-STAR’s structure allows manufacturers to present data in a way that aligns with FDA’s review needs. Manufacturers should take advantage of this by thoroughly organizing clinical data, using appendices as necessary to ensure clarity and depth. - Utilizing Real-Time Validation and Checks
By leveraging e-STAR’s real-time validation and error-checking, manufacturers can minimize potential errors that could otherwise lead to costly and time-consuming delays. - Device-Specific Risk Management Documentation
PMA submissions should include device-specific risk management data. Manufacturers should consider device-specific factors and potential patient scenarios in their risk analysis, ensuring that e-STAR’s risk management fields fully capture the device’s safety profile.
e-STAR’s Contribution to Streamlining PMA Processes
e-STAR has redefined PMA submissions by addressing the key challenges manufacturers face with Class III devices. The tool’s structured templates reduce complexity, improve accuracy, and support efficient data review, making the PMA process more manageable for manufacturers and review teams alike.
- Enhanced Submission Quality
e-STAR’s structured format promotes high submission quality by guiding manufacturers through each necessary data component. This reduces the likelihood of errors and missing information, resulting in a smoother FDA review process. - Consistency Across Submissions
e-STAR standardizes PMA submissions, improving consistency across applications. This allows FDA reviewers to analyze data more quickly and make informed decisions with greater confidence, especially when dealing with devices involving new technology or unique functionality. - Potential for Reduced Approval Times
By organizing data in line with FDA requirements and reducing the likelihood of RAIs, e-STAR can potentially shorten PMA review timelines. This streamlined approach enables manufacturers to bring Class III devices to market faster, providing life-saving technologies to patients more efficiently.
Example of Improved Efficiency with e-STAR
A mid-sized company developed a new neurostimulator for chronic pain management. With e-STAR, they compiled clinical data, preclinical studies, and risk assessments in a structured format. The standardized presentation helped FDA reviewers assess safety and efficacy quickly, resulting in an approval timeline shorter than the typical PMA process.
Conclusion
The e-STAR program has introduced transformative efficiencies in PMA submissions for Class III devices. Through standardized templates, automated error-checking, and designated fields for essential data, e-STAR supports manufacturers in meeting FDA’s rigorous requirements for high-risk devices. With organized documentation, reduced errors, and improved clarity, e-STAR helps expedite FDA’s review process, enabling faster patient access to critical medical technologies. For manufacturers, leveraging e-STAR for PMA submissions can streamline the path to market, ensuring that their life-sustaining and high-risk devices meet regulatory standards without unnecessary delays.
Summary and Best Practices for e-STAR Submissions
A successful e-STAR submission starts with a thorough understanding of FDA requirements and the specific documentation necessary for the type of device being submitted. Each classification (Class I, II, or III) has unique requirements that determine the content and format of the submission.
- Review FDA Guidelines for Device Classification
Start by confirming the device classification to determine the appropriate submission type: 510(k), De Novo, or PMA. Understanding the risk level of the device and its classification helps in identifying essential documentation, including clinical data, performance testing, and risk assessments. - Identify Required Documentation Based on Submission Type
- 510(k) Submissions
Focus on demonstrating substantial equivalence to a predicate device, including comparative data and labeling. - De Novo Submissions
Provide detailed safety and efficacy data for novel devices without a predicate, focusing on clinical and performance testing. - PMA Submissions
Include comprehensive preclinical and clinical data to demonstrate safety and effectiveness, as well as quality system compliance.
- 510(k) Submissions
- Assemble Data for Clinical and Preclinical Studies
For Class II and III devices, clinical data is often required. Collect all relevant clinical study data, performance testing results, and laboratory data early in the process to ensure a comprehensive submission. - Conduct a Pre-Submission Meeting with FDA
Pre-submission meetings allow manufacturers to clarify data requirements with FDA reviewers, reducing the likelihood of requests for additional information (RAIs). These meetings are especially beneficial for novel devices and complex PMA submissions.
2. Organizing and Compiling Essential Documents
A well-organized submission package is crucial for a smooth FDA review. e-STAR’s structured format is designed to help manufacturers organize their documentation efficiently, ensuring each section is completed accurately.
- Device Description and Intended Use
- Clearly define the device’s purpose, key functionalities, and intended use. Ensure consistency in terminology and descriptions across all sections.
- Include specifications, design details, and a description of how the device operates to ensure FDA reviewers have a clear understanding of the device.
- Labeling and Instructions for Use
Labeling should reflect the intended use, target population, and any critical safety information. Use the e-STAR template’s labeling sections to highlight important information, including warnings, contraindications, and operating instructions. - Risk Management Documentation
- For devices requiring risk management data, provide a detailed hazard analysis and risk assessment, including identified risks and mitigation strategies.
- Use e-STAR’s risk management fields to describe how the device meets safety standards and reduces user risk.
- Performance and Safety Testing Data
- Compile performance testing results, including biocompatibility testing, electrical safety, and mechanical testing.
- Ensure that all testing data is documented accurately, with clear references to FDA guidance documents and industry standards.
3. Completing the e-STAR Template Accurately
The e-STAR template is designed to guide users through the submission requirements for each device class, using structured fields and built-in prompts. Completing the template accurately requires attention to detail and a systematic approach.
Data Entry Best Practices
- Follow Section Prompts
Each section of e-STAR includes prompts to guide data entry. Follow these prompts closely, as they ensure all necessary information is provided and organized in alignment with FDA expectations.
- Use Clear, Concise Language
- Use concise language when describing technical details to prevent misunderstandings. Avoid overly complex jargon and explain technical terms where necessary.
- Provide summaries or explanations for complex data to facilitate the FDA’s understanding of the submission.
- Avoid Redundant Information
Repetition can clutter the submission and increase the chance of inconsistencies. Enter data in the relevant sections only and cross-reference where needed to keep the submission organized. - Cross-Check for Consistency
Consistent data is crucial for regulatory submissions. Verify that information, such as device specifications and intended use, matches across all sections of the e-STAR template.
Using Error-Checking Features
e-STAR’s automated error-checking is invaluable for identifying missing or inconsistent information. Use this feature as part of the final review to ensure that all fields are completed accurately before submission.
- Run Validation Checks Regularly
Validation checks should be run periodically during the submission process, not just at the end. This helps catch errors early, making it easier to correct them before finalizing the document. - Resolve Flagged Errors Promptly
Address any flagged errors as soon as possible to avoid delays in submission. These errors can include missing data, incomplete sections, or formatting inconsistencies.
4. Adhering to FDA’s e-STAR Protocols for Efficient Review
Staying within FDA protocols ensures that the submission process proceeds smoothly, with fewer RAIs and a greater chance of timely approval.
- Follow FDA’s Latest Guidance Documents
FDA regularly updates guidance documents and standards for different device classes. Ensure that your submission aligns with the latest guidance, particularly for performance standards, testing protocols, and clinical data requirements.
- Document Compliance with Relevant Standards
- Include references to FDA-recognized consensus standards in your submission. These standards help FDA reviewers assess whether the device meets safety and performance requirements.
- Provide certificates of conformity, where applicable, to support claims of compliance with industry standards.
- Double-Check Submission for Completeness
Ensure that all necessary fields are filled out and that the submission is as complete as possible. Incomplete submissions are the primary cause of RAIs, which delay the review process.
Pre-Submission Considerations
- Request a Pre-Submission Review (if applicable)
For complex devices, a pre-submission review can clarify expectations, reducing the likelihood of time-consuming feedback and allowing manufacturers to align their data with FDA’s requirements. - Update Documents for Submission Consistency
Before submitting, ensure that any updated data (e.g., newly conducted tests) is reflected throughout the submission. Inconsistent or outdated data can lead to confusion and potential delays.
5. Best Practices for Common e-STAR Submission Types
The specific requirements for 510(k), De Novo, and PMA submissions vary. Here are best practices for each type to ensure a successful submission process.
Best Practices for De Novo Submissions
- Document Safety and Effectiveness Thoroughly
Since De Novo devices lack a predicate, comprehensive evidence of safety and effectiveness is required. Use e-STAR to present clear, detailed data that addresses all aspects of device safety. - Provide Clear Risk Analysis
Without a predicate, risk analysis plays a critical role in De Novo submissions. e-STAR’s risk management sections should include a complete hazard analysis and risk mitigation strategies. - Pre-Submission Feedback
De Novo submissions benefit greatly from pre-submission consultations to clarify safety and efficacy expectations. This reduces the chance of RAIs and provides alignment with FDA’s standards for new technologies.
Best Practices for PMA Submissions
- Organize Clinical and Preclinical Data
PMA applications require substantial clinical and preclinical data, which should be well-organized in e-STAR’s structured fields to facilitate efficient review. - Ensure Quality System Compliance Documentation
For PMA submissions, demonstrate adherence to Quality System Regulations (QSR) with relevant documentation. e-STAR’s templates support QSR documentation, reducing the need for additional FDA inquiries. - Highlight Risk-Benefit Analysis
Risk-benefit analysis is critical for PMA submissions. Use e-STAR to document potential risks, mitigation strategies, and evidence that the benefits of the device outweigh its risks.
6. Conducting a Final Review and Preparing for Submission
A final, comprehensive review of the e-STAR submission package is essential before sending it to the FDA.
- Conduct an Internal Review
Have a team member not involved in the preparation process review the submission. A fresh perspective can help catch any errors or inconsistencies missed during initial reviews. - Ensure All Required Attachments Are Included
Confirm that all supplementary documents, such as testing reports, certificates, and compliance documentation, are attached in the correct e-STAR sections. - Run a Final Validation Check
Use e-STAR’s validation feature one last time to confirm that there are no missing fields, errors, or inconsistencies. - Submit and Prepare for Potential FDA Feedback
After submission, be prepared to respond quickly to any questions or requests from the FDA. Having clear, organized documentation available for follow-up is essential for addressing inquiries efficiently.
Benefits for Regulatory Professionals and Manufacturers
Reduced Review Times
The structured e-STAR format significantly reduces FDA review times by eliminating many bottlenecks in the traditional submission process. This accelerated process helps manufacturers get their devices to market faster, which can be particularly valuable for high-demand devices that address urgent public health needs, such as diagnostic tools or emergency medical equipment. For regulatory professionals, e-STAR’s clear, structured approach reduces the number of resubmissions and additional document requests, providing an overall faster route to clearance or approval (FDA, 2023f).
- Efficiency in Submission Preparation
With pre-formatted fields, checklists, and step-by-step guidance, e-STAR streamlines document preparation, allowing even small regulatory teams to handle the process effectively without extensive outside resources. This is especially beneficial for startups and smaller firms with limited regulatory expertise, as it minimizes the need for specialized consultants and allows in-house teams to take the lead (Shuren, 2023). - Minimizing Costly Delays
Any delay in the submission process can have significant cost implications, particularly for startups with limited budgets. The real-time feedback and validation provided by e-STAR reduce the chances of RAIs, cutting down on the time and resources spent on document corrections and re-submissions. For manufacturers, these reduced delays not only lower costs but also allow them to capitalize on early market entry, enhancing their competitive positioning (FDA, 2023g).
Accurate and complete data submissions are crucial for regulatory success. e-STAR’s automated error-checking capabilities ensure that submissions meet FDA requirements by identifying omissions, inconsistencies, or formatting errors prior to submission. This validation feature not only improves data quality but also gives regulatory professionals confidence that their applications align with FDA standards on the first try, reducing the likelihood of rejected or delayed submissions (Smith & Johnson, 2023).
- Reducing Human Error
By automating data validation, e-STAR minimizes human error, which is a common issue in manual submission processes. This is especially important for sections like clinical data reporting and risk management documentation, where accuracy is paramount. With e-STAR’s guidance, regulatory teams can focus on the content of their submissions without being bogged down by formatting or minor technicalities (U.S. Department of Health and Human Services, 2023). - Supporting Smaller Manufacturers
For smaller manufacturers with limited resources, e-STAR offers a structured, accessible platform that simplifies compliance. These companies often face challenges in navigating FDA regulations due to limited budgets and staff, making e-STAR’s guidance particularly valuable. The structured approach allows these companies to confidently submit compliant applications, potentially avoiding costly delays and accelerating their path to market (Patel, 2022).
The FDA’s e-STAR program has brought a transformative impact to the premarket submission process, offering streamlined, standardized, and efficient templates that benefit both regulatory professionals and medical device manufacturers. By simplifying document preparation, reducing review times, and ensuring data quality, e-STAR supports the FDA’s mission of safeguarding public health while enabling timely access to innovative medical devices. The continued adoption of e-STAR is anticipated to drive greater consistency and predictability in FDA’s review process, benefiting industry stakeholders and patients alike.
e-STAR Templates for the following medical devices can be found here.
| Requirement |
| 510(k), De Novo, and PMA4: medical device submissions for Non-In Vitro Diagnostic devices |
| 510(k), De Novo, and PMA medical device submissions for In Vitro Diagnostic devices |
| Pre-Submissions and 513(g) requests for information for Non-In Vitro and In Vitro Diagnostic |
Conclusion: Leveraging e-STAR for a Successful Submission
By following these best practices, manufacturers can maximize the effectiveness of their e-STAR submissions. From initial document compilation to final review, e-STAR provides a framework that supports efficient, accurate, and compliant submissions. By adhering to these guidelines, manufacturers can improve their chances of a smooth FDA review process, ultimately bringing safe, effective medical devices to market in a timely manner.
